In the world of healthcare, getting paid isn’t as simple as handing over a bill. Instead, providers must navigate the insurance claims process — a detailed and sometimes frustrating path that stretches from patient registration to reimbursement.
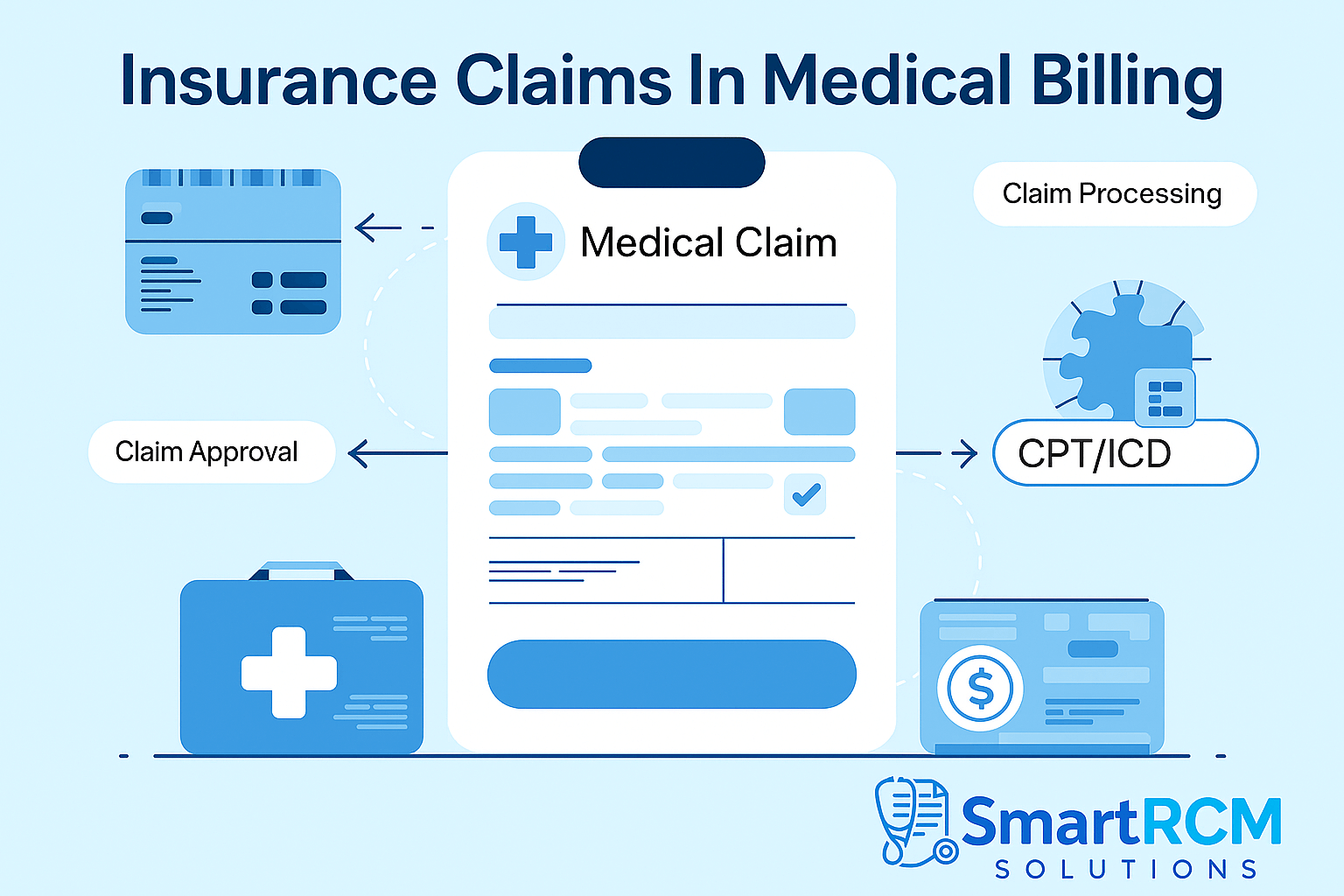
Insurance Claims In Medical Billing
Whether you’re a medical biller, clinic manager, or healthcare provider, understanding each stage of this journey is crucial for minimizing delays, reducing denials, and maintaining a healthy revenue cycle.
This comprehensive guide breaks down every step of the process, from claim creation to payment, while highlighting common pitfalls and best practices.
📌 What is an Insurance Claim?
An insurance claim is a formal request sent by a healthcare provider to a patient’s insurance company, asking for reimbursement for medical services rendered.
It includes:
- Patient information
- Diagnosis codes (ICD-10)
- Procedure codes (CPT/HCPCS)
- Provider details
- Service dates and costs
🧭 Step-by-Step: How an Insurance Claim Moves Through the System
1. Patient Registration and Verification
Before the claim process even begins, it’s vital to collect accurate:
- Demographic information (name, DOB, address)
- Insurance details (payer name, policy number, group number)
👉 Tip: Always verify insurance eligibility before the appointment to avoid coverage issues later.
2. Coding the Encounter
After a provider sees the patient, medical coders assign:
- ICD-10 codes for diagnoses
- CPT/HCPCS codes for procedures and services
These codes form the foundation of the claim and must be accurate and compliant.
3. Claim Creation
Using practice management software, the biller creates a claim with all required information:
- Provider NPI and Tax ID
- Place of service
- Referring provider (if applicable)
- Service dates and charges
The claim can be electronic (837P or 837I) or paper (CMS-1500 or UB-04).
4. Claim Submission
The claim is then submitted to the insurance payer, usually via a clearinghouse.
Clearinghouses:
- Check claims for basic errors (scrubbing)
- Convert data into payer-compatible formats
- Forward claims to insurance companies
5. Adjudication by the Insurance Company
The insurance payer reviews the claim in a process called adjudication, where they:
- Validate the codes and coverage
- Check medical necessity
- Determine payment amount
They may:
✅ Approve the claim
❌ Deny it (with reasons)
🔁 Request more information
Read More: Medical Billing Compliance Checklist for 2025
6. Payment or Denial
Once adjudication is complete:
- A payment is issued to the provider or assigned party
- An Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA) is sent, outlining:
- Amount billed
- Amount paid
- Patient responsibility
- Adjustments or denials
7. Posting Payment in the System
Billers post the payment details into the practice’s billing system to update the account. This is important for:
- Tracking revenue
- Managing patient balances
- Reporting financial performance
8. Follow-up or Appeal (if needed)
If the claim is denied or underpaid:
- The biller must review the EOB/ERA
- File an appeal with supporting documents
- Re-submit the corrected claim
📌 Note: Timely follow-ups can recover thousands in missed revenue.
🛠️ Common Reasons for Claim Denials
Even experienced billers encounter denials. Here are the most common causes:
| Reason | Explanation |
|---|---|
| Incorrect patient info | Misspelled name, wrong DOB, or outdated insurance |
| Invalid or missing codes | ICD or CPT codes are outdated or mismatched |
| Lack of prior authorization | Services rendered without required payer approval |
| Duplicate claim | Claim already submitted for the same service/date |
| Non-covered services | Procedure not included in the patient’s plan |
✅ Best Practices for Smooth Claim Processing
- Always verify eligibility before appointments
- Use clearinghouses to detect early errors
- Keep coding and documentation compliant
- Train staff on payer-specific rules
- Follow-up on unpaid claims every 14–21 days
- Stay current with insurance policies and code updates
Read More: What Is Prior Authorization in Medical Billing?
📈 Why Understanding the Claims Process Matters
Efficient claim handling leads to:
- Faster payments
- Fewer denials
- Happier patients
- Healthier cash flow
For clinics and billing teams, this knowledge empowers smarter workflows and better financial results.
❓ Frequently Asked Questions (FAQs)
Q1. What’s the difference between a denied and rejected claim?
A: A rejected claim has errors and never reached the payer’s adjudication system. A denied claim was reviewed but not approved for payment.
Q2. How long does it take to get paid after submitting a claim?
A: Most payers process claims within 7 to 30 days, depending on accuracy and contract terms.
Q3. Can patients be billed after insurance pays?
A: Yes. After the insurance pays its portion, the remaining balance (co-pay, deductible, or co-insurance) can be billed to the patient.
Q4. What is an ERA?
A: An Electronic Remittance Advice is a digital version of the Explanation of Benefits sent by the payer showing how the claim was processed.
Q5. Can I resubmit a denied claim?
A: Yes. You can file a corrected claim or appeal, depending on the reason for denial.
🧠 Final Thoughts
Mastering the insurance claims process is essential for every medical billing professional. From submission to payment, understanding each step allows you to reduce delays, minimize rejections, and improve your practice’s financial performance.