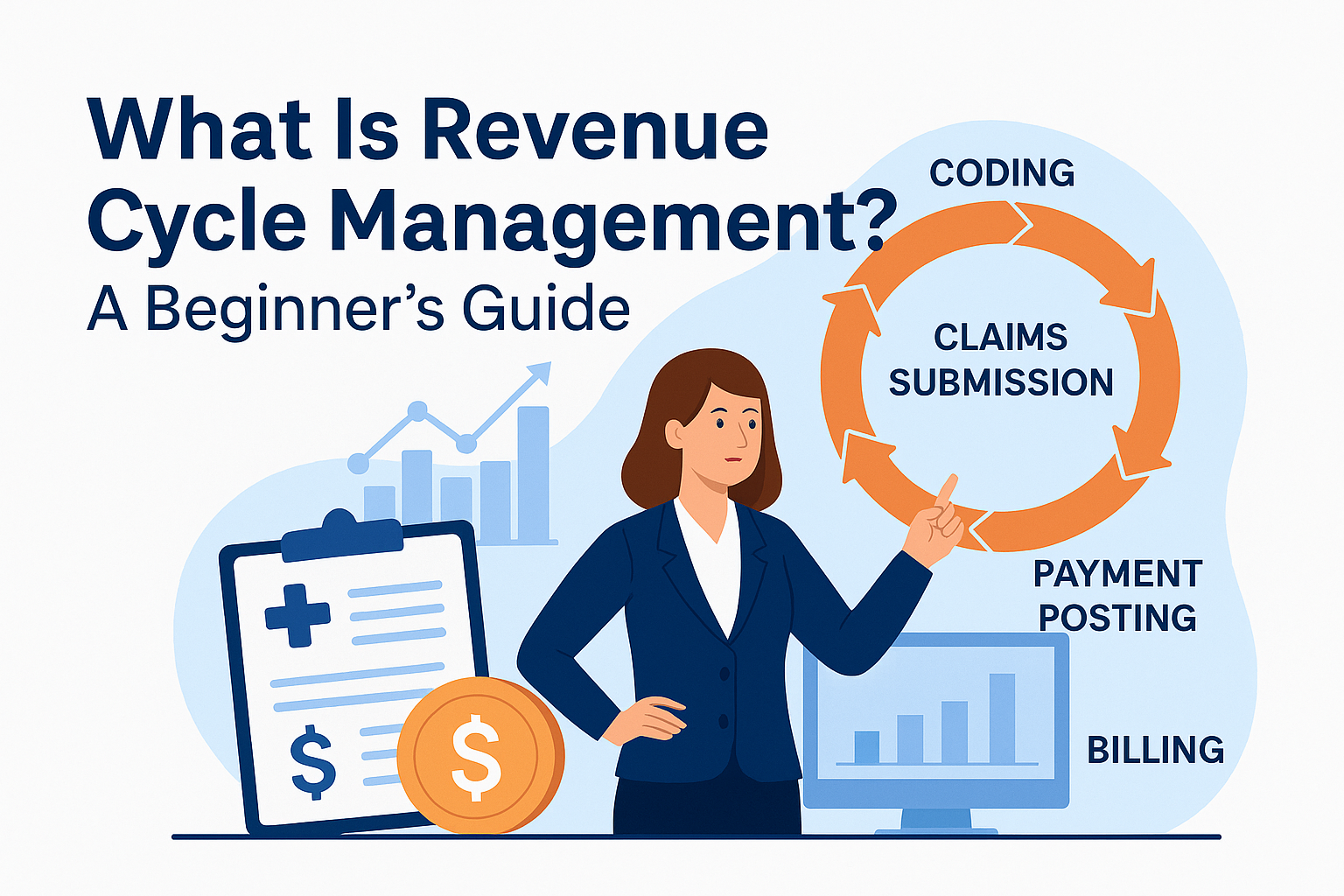
RCM is the financial process used by healthcare organizations to track patient care episodes from registration and appointment scheduling to the final payment of a balance. In this guide, we will walk you through the Revenue Cycle Management (RCM) process step by step, helping your healthcare practice improve efficiency, reduce errors, and increase revenue. Whether you’re a small clinic or a large healthcare facility, following these best practices will ensure smoother operations and faster payments.

What Is Revenue Cycle Management (RCM)?
Revenue Cycle Management (RCM) is the process used by healthcare systems to manage the financial aspects of patient services. It begins the moment a patient schedules an appointment and ends once all claims and payments have been processed. The goal of RCM is to identify, collect, and manage revenue from payers and patients efficiently.
In simpler terms, RCM is how healthcare providers get paid for the services they deliver.
Key Steps in the RCM Process
Here we have listed the steps of RCM.

1. Patient Scheduling and Registration
The cycle begins when a patient calls or books an appointment. During registration, accurate demographic and insurance information is collected, including name, date of birth, insurance ID, and policy details. Accurate registration is vital to avoid downstream billing errors.
2. Eligibility and Insurance Verification
This step ensures the patient’s insurance is active and covers the services scheduled. Real-time verification tools help identify coverage gaps, copayments, deductibles, and prior authorization needs before services are rendered.
3. Charge Capture
Charge capture is the process of recording the services provided to the patient. It typically involves using medical codes (CPT, HCPCS) that align with the care given during a visit or procedure.
4. Medical Coding
Medical coders translate provider notes and clinical documentation into standard codes (ICD-10, CPT, etc.). These codes determine how a claim will be processed and reimbursed.
5. Charge Entry
The charges are entered into the medical billing software using the coded data. This includes linking diagnosis codes with appropriate procedure codes and applying any necessary modifiers.
6. Claim Submission
Once coded and reviewed, claims are submitted electronically to insurance companies or government payers like Medicare and Medicaid. Clean claims reduce delays and rejections.
7. Payment Posting
Payments received from insurance companies and patients are posted against each claim. This step allows healthcare providers to track which payments have been made, denied, or are still outstanding.
8. Denial Management
If a claim is denied, the biller investigates the reason and corrects the issue before resubmitting the claim. Effective denial management helps maintain steady cash flow and avoid write-offs.
9. Patient Collections
After insurance has paid its share, patients are billed for the remaining balance. This step may involve sending statements, setting up payment plans, or following up on overdue accounts.
Why Revenue Cycle Management Is Important
An efficient RCM process improves both financial performance and patient satisfaction. Here’s why it matters:
-
Reduces claim denials and rework
-
Improves cash flow and revenue predictability
-
Enhances operational efficiency
-
Ensures regulatory and payer compliance
-
Provides accurate financial reporting
Common Challenges in RCM
Despite its importance, RCM is often affected by challenges such as:
-
Inaccurate patient registration
-
Delays in coding or billing
-
Outdated or poorly integrated software
-
High denial rates
-
Lack of staff training or resources
-
Inefficient follow-up on accounts receivable
Best Practices for Effective RCM
-
Use Integrated Software Systems:
Choose EHR and billing systems that are seamlessly connected to eliminate data silos. -
Regular Staff Training:
Ensure your front office, coders, and billers are up to date on changes in payer policies and compliance rules. -
Automate Where Possible:
Automate tasks like eligibility checks, payment reminders, and claims submission to reduce errors. -
Track KPIs Regularly:
Monitor performance indicators like days in AR, denial rates, and clean claim rates. -
Focus on Clean Claims:
Ensure every claim is reviewed and validated before submission to minimize rejections and rework. -
Patient Transparency:
Provide patients with upfront cost estimates and clear billing communication to improve collections and trust.
How Outsourcing Can Help
Many healthcare providers outsource their RCM processes to medical billing companies for better efficiency and compliance. Outsourcing can help:
-
Reduce staffing overhead
-
Increase revenue through better denial management
-
Ensure billing is done accurately and on time
-
Allow providers to focus on patient care

Conclusion:
Revenue Cycle Management is not just a financial tool—it’s a strategic asset that ensures the long-term success of healthcare practices. From patient registration to final collections, every step must be carefully managed to optimize reimbursement and minimize delays. By following best practices, using modern tools, and continuously training your team, you can build a robust RCM process that supports both operational and financial goals. If you’re considering outsourcing your RCM, Smart RCM Solutions offers expert services at affordable rates. We specialize in helping practices like yours improve cash flow, reduce claim denials, and focus more on patient care while we handle the complexities of the revenue cycle.